A herniated disc can cause intense back pain, numbness, and weakness, making everyday activities challenging. Whether it’s due to aging, poor posture, or a sudden injury, this condition affects millions of people worldwide. The good news? Most cases can be managed with the right combination of treatment, exercises, and lifestyle changes—without the need for surgery.
In this guide, we’ll cover everything you need to know about herniated discs, including their causes, symptoms, best treatment options, and exercises to help you recover faster. Let’s dive in!
Table of Contents
📢 Before you continue: Sign up below for home recovery tips, injury rehab advice, and therapist-approved gear reviews straight to your inbox!!
🏁 What Is a Herniated Disc?
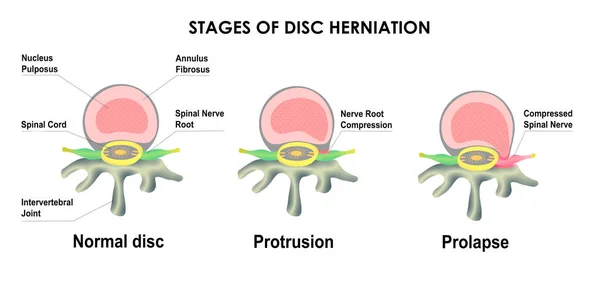
A herniated disc occurs when the soft inner core of a spinal disc pushes through the tough outer layer. This can irritate nearby nerves, leading to pain, weakness, or numbness.
How a Herniated Disc Develops
- The spine is made up of vertebrae separated by intervertebral discs, which act as shock absorbers.
- Over time or due to injury, a disc can bulge, rupture, or herniate, pressing on nerves and causing pain.
Common Locations of a Herniated Disc
- Cervical spine (neck) – Can cause pain in the shoulders, arms, and hands.
- Lumbar spine (lower back) – The most common area, often leading to sciatica (radiating leg pain).
- Thoracic spine (mid-back) – Rare but possible.
🧾 Causes and Risk Factors
Common Causes
- Aging – Natural wear and tear (disc degeneration) makes discs more prone to herniation.
- Injury or Trauma – A sudden movement, fall, or accident can rupture a disc.
- Improper Lifting – Lifting heavy objects with poor form can put excessive stress on the spine.
- Repetitive Strain – Frequent bending, twisting, or prolonged sitting can weaken discs.

Risk Factors
- Sedentary Lifestyle – Lack of movement leads to weaker back muscles.
- Excess Weight – Extra body weight increases spinal pressure.
- Smoking – Reduces blood flow to spinal discs, accelerating degeneration.
- Genetics – A family history of spinal conditions may increase risk.
🟡 Signs and Symptoms
A herniated disc can cause a variety of symptoms depending on its location in the spine. Some people experience mild discomfort, while others suffer from severe pain, numbness, or weakness. Recognizing the signs early can help in getting the right treatment before symptoms worsen.
1. Common Symptoms of a Herniated Disc
The symptoms of a herniated disc depend on whether it occurs in the cervical (neck), thoracic (mid-back), or lumbar (lower back) spine.
A. Herniated Disc in the Neck (Cervical Spine)
When a herniated disc presses on nerves in the neck, it may cause:
✅Neck pain that may spread to the shoulders and arms.
✅Numbness or tingling in the arms, hands, or fingers.
✅Weakness in the arms or trouble gripping objects.
✅ Headaches in some cases.
B. Herniated Disc in the Lower Back (Lumbar Spine)
A herniated disc in the lower back is more common and may cause:
✅Lower back pain that worsens with movement.
✅ Sciatica – sharp pain radiating down the leg, often to the foot.
✅Numbness or tingling in the buttocks, legs, or feet.
✅Muscle weakness affecting walking or standing.
C. Herniated Disc in the Mid-Back (Thoracic Spine) – Rare but Serious
Although rare, a herniated disc in the mid-back can cause:
✅ Upper or mid-back pain that may wrap around the chest.
✅ Difficulty breathing if the nerves affecting the lungs are involved.
✅Loss of bladder or bowel control (seek medical help immediately).
2. Severe Symptoms That Require Immediate Medical Attention
In rare cases, a herniated disc can cause dangerous symptoms, such as:
🚨 Loss of bladder or bowel control – May indicate cauda equina syndrome, a medical emergency.
🚨 Severe, progressive weakness in the legs or arms.
🚨 Numbness in the inner thighs or buttocks (saddle anesthesia).
3. How Symptoms Change Over Time
- Mild cases: Symptoms may improve within a few weeks with rest and treatment.
- Moderate cases: Ongoing pain and discomfort may require physical therapy.
- Severe cases: If symptoms persist or worsen, advanced treatments like injections or surgery may be needed.
🧑⚕️ How Is a Herniated Disc Diagnosed?
Diagnosing a herniated disc involves a combination of medical history, physical examination, and imaging tests. Since symptoms can vary depending on the location and severity of the disc issue, doctors use different methods to confirm the diagnosis and rule out other conditions.
1. Medical History and Symptom Assessment
The first step in diagnosing a herniated disc is discussing your symptoms, medical history, and lifestyle habits. A doctor may ask:
- When did the pain start?
- Does the pain radiate to other areas, like the arms or legs?
- What movements or activities make it worse?
- Have you had previous back or neck injuries?
2. Physical Examination
A physical exam helps identify nerve involvement and mobility issues. The doctor may check for:
- Pain response when pressing on the spine.
- Reflexes and muscle strength to detect nerve compression.
- Range of motion tests to assess stiffness or movement limitations.
- Sensory tests to check for numbness or tingling.
Straight Leg Raise Test (For Lumbar Herniated Discs)

A common test for lower back herniated discs involves:
- Lying on your back while the doctor lifts one leg straight.
- If pain occurs between 30-70 degrees, it may indicate nerve irritation from a herniated disc.
3. Imaging Tests for a Definitive Diagnosis
If symptoms suggest a herniated disc, imaging tests help confirm the condition and rule out other spinal problems.
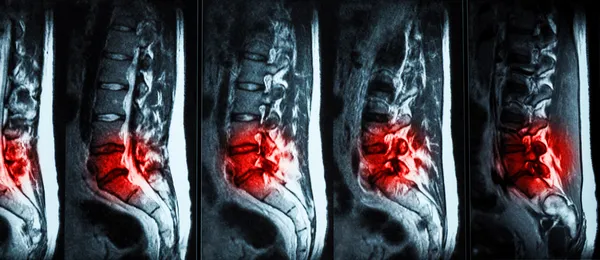
A. MRI (Magnetic Resonance Imaging) – Most Common Test
- Why it’s used: Provides detailed images of soft tissues, including discs and nerves.
- What it shows: Disc herniation, nerve compression, and inflammation.
B. CT Scan (Computed Tomography) with Myelogram
- Why it’s used: Helps visualize the spinal canal and nerve compression.
- When it’s used: If an MRI isn’t available or if more detail is needed.
C. X-Ray – Rules Out Other Issues
- Why it’s used: Shows spinal alignment and detects fractures but does not show soft tissue like discs.
4. Nerve Function Tests (If Needed)
If nerve damage is suspected, additional tests may be performed:
A. Electromyography (EMG) and Nerve Conduction Studies (NCS)
- Why it’s used: Measures nerve signals to check for damage.
- When it’s used: If symptoms suggest severe nerve compression or weakness.
When to See a Doctor
Seek medical attention if you experience:
✅Severe or worsening pain that doesn’t improve with rest.
✅ Numbness, tingling, or weakness in the arms or legs.
✅Loss of bladder or bowel control (a medical emergency).
💊 Best Treatment Options for a Herniated Disc
The treatment for a herniated disc depends on the severity of symptoms. Many people recover with conservative treatments, while others may need medical interventions or, in rare cases, surgery. Below are the best treatment options to relieve pain and improve spinal health.
Conservative Treatments
- Rest & Activity Modification – Avoid strenuous activities but stay mobile.
- Ice & Heat Therapy – Ice for inflammation, heat for muscle relaxation.
- Pain Medications – NSAIDs (ibuprofen), muscle relaxants, or steroid injections.
Physical Therapy & Alternative Treatments
- Physical Therapy – Strengthening and stretching exercises help recovery.
- Chiropractic Care – May provide relief but should be used cautiously.
- Acupuncture & Massage Therapy – Can help with pain relief.
When Surgery Is Necessary
- Microdiscectomy – Removes the herniated portion of the disc.
- Spinal Fusion – Fuses vertebrae to stabilize the spine.
- Artificial Disc Replacement – An alternative to fusion in some cases.

🏋️ Best Exercises for a Herniated Disc
Exercise plays a crucial role in the recovery and management of a herniated disc. The right movements can help reduce pain, improve flexibility, and strengthen the muscles supporting the spine. However, improper exercises or excessive strain can make symptoms worse. Experts recommend starting with gentle physical therapy exercises for herniated disc recovery at home to restore mobility safely. Below are the best exercises for a herniated disc, focusing on relief and long-term spinal health.
1. Stretching Exercises for Pain Relief
Gentle stretching helps reduce stiffness and relieves pressure on the herniated disc by improving spinal mobility.
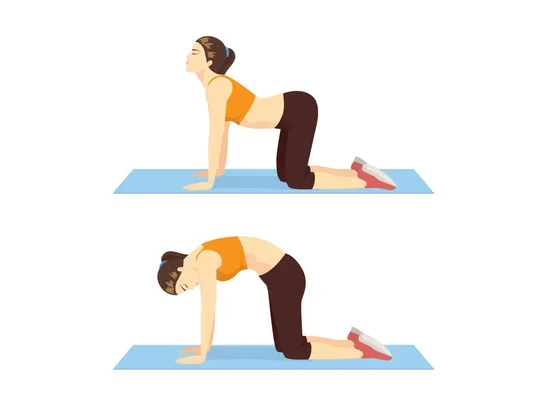
A. Cat-Cow Stretch
Benefits: Improves spinal flexibility and relieves lower back tension.
How to do it:
- Get on all fours with your hands under your shoulders and knees under your hips.
- Inhale, arch your back, and lift your head (Cow Pose).
- Exhale, round your back, and tuck your chin (Cat Pose).
- Repeat slowly for 8-10 reps.
B. Child’s Pose
Benefits: Stretches the lower back and decompresses the spine.
How to do it:
- Kneel on the floor and sit back on your heels.
- Extend your arms forward and rest your forehead on the ground.
- Hold for 20-30 seconds and repeat 2-3 times.

2. Strengthening Exercises for Core and Back Support
A strong core helps support the spine and reduces the strain on a herniated disc.
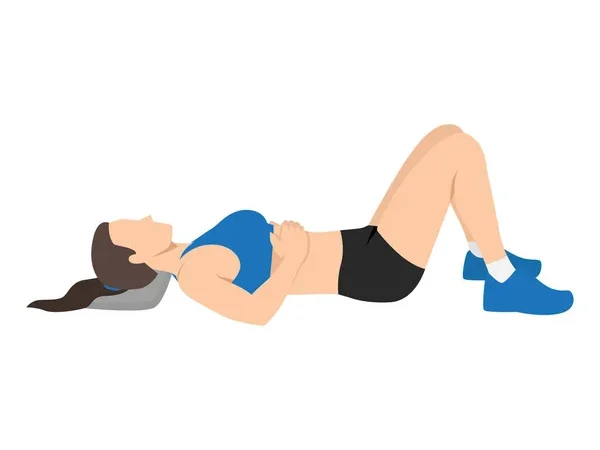
A. Pelvic Tilts
Benefits: Strengthens the core and stabilizes the lower back.
How to do it:
- Lie on your back with knees bent and feet flat on the floor.
- Tighten your abdominal muscles and press your lower back into the floor.
- Hold for 5 seconds, then release.
- Repeat 10-12 times.
B. McKenzie Extensions
Benefits: Helps reposition the herniated disc and relieves pressure on nerves.
How to do it:
- Lie face down on the floor with hands under your shoulders.
- Push up gently, extending your back while keeping hips on the ground.
- Hold for 5 seconds, then lower back down.
- Repeat 8-10 times.

3. Low-Impact Aerobic Activities
Aerobic exercise improves circulation, promotes healing, and keeps the spine flexible.
A. Walking
- Why it helps: Low-impact, keeps the spine moving without excessive strain.
- Tip: Maintain good posture and avoid uneven surfaces.
B. Swimming or Water Therapy
- Why it helps: The buoyancy reduces spinal pressure while improving strength and flexibility.
- Tip: Try water walking or gentle backstroke for safe movement.
4. Exercises to Avoid with a Herniated Disc
Some movements can worsen a herniated disc and should be avoided:
🚫 Heavy weightlifting (deadlifts, squats, overhead presses)
🚫 Deep forward bends (touching toes, full sit-ups)
🚫 Twisting movements (golf swings, Russian twists)
Final Tips for Exercising with a Herniated Disc
✅ Start with gentle stretches and progress slowly.
✅ Focus on low-impact exercises and avoid sudden movements.
✅ Listen to your body—stop if pain increases.
✅ Consider physical therapy for a personalized rehab plan.
By incorporating these herniated disc-friendly exercises, you can improve mobility, strengthen your spine, and reduce pain over time.
🏆 Prevention and Future Flare-Ups
Posture and Ergonomics
- Maintain proper sitting posture at work.
- Use lumbar support when sitting for long hours.
Safe Lifting Techniques
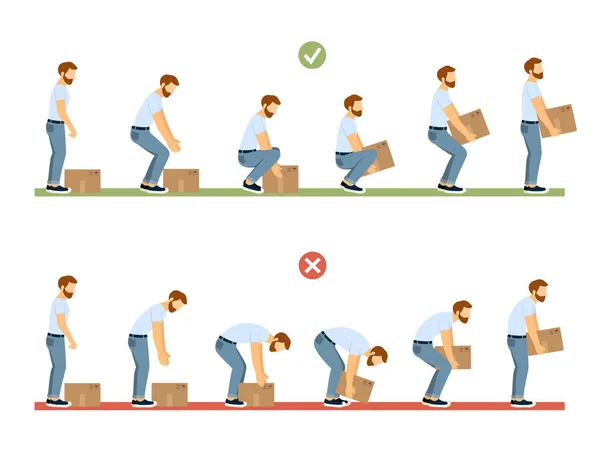
- Keep a straight back and lift with your legs.
- Avoid twisting while lifting heavy objects.
Long-Term Spine Health Tips
- Stay active with low-impact exercises (walking, swimming).
- Strengthen core muscles to support the spine.
- Use ergonomic rehab tools like back braces and foam rollers.
✅ Conclusion
A herniated disc can cause significant discomfort, but with the right approach, most people can manage their symptoms and recover without surgery. Understanding the causes, symptoms, and treatment options is key to making informed decisions about your spinal health.
If you’re dealing with a herniated disc, start with conservative treatments like rest, physical therapy, and targeted exercises. Physical therapists often recommend simple daily stretches for herniated disc pain relief at home to manage symptoms safely. Avoid movements that worsen symptoms and focus on proper posture and spine-friendly habits to prevent future flare-ups.
For those experiencing severe or persistent pain, consulting a healthcare provider is essential to explore options like pain management techniques, injections, or surgical interventions if necessary.
By staying proactive with exercise, spine care, and ergonomic adjustments, you can protect your back and reduce the risk of further disc issues.
🚀 Looking for the best home rehab equipment to support your herniated disc recovery? Check out our top recommendations below!
| Product | Description | Why It Helps | Affiliate Link |
|---|---|---|---|
| Home Lumbar Traction Kit | Portable device that gently stretches the lower back to reduce disc pressure. | Helps create space between vertebrae, relieving nerve compression caused by herniated discs. | 🔗Shop on Amazon |
| Spinal Decompression Harness | Harness system used with a doorway or bar to apply vertical traction to the spine. | Provides spinal unloading and gentle decompression, reducing disc pressure and nerve irritation. | 🔗Shop on Amazon |
| TENS Unit | Electrical stimulation device with adjustable intensity and pre-set programs. | Blocks pain signals and stimulates endorphin release to reduce herniated disc pain non-invasively. | 🔗Shop on Amazon |
| Heating Pad | Soft, adjustable heating pad with multiple heat settings and auto shut-off. | Relaxes tight muscles, improves circulation, and supports healing in the lower back. | 🔗Shop on Amazon |